
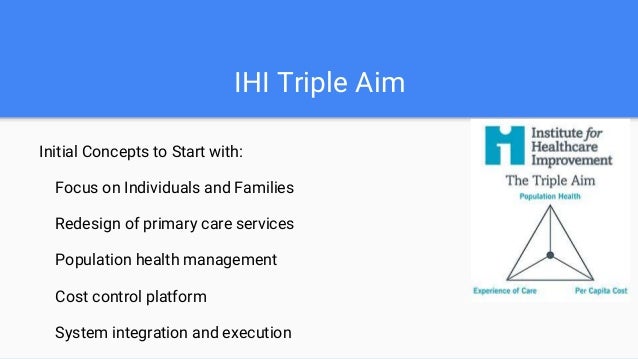
Although the transition from a fee-for-service to value-based payment delivery models has been slow, the healthcare landscape will continue to evolve, and physicians will adopt value-based care models in their practices.What is the triple aim, and how can we slow down the rising cost of care? These services reduce the administrative burden of quality data submissions and audits, making it easier to avoid payment adjustments for failing to submit data. Once you have successfully captured all the clinical data that CMS requires, work with your PM/EMR vendor to submit your individual provider or group practice quality data directly to CMS. Link to individual patient records as proof points.More readily focus on the measures that need improvement.View weekly measurement updates to help identify problem areas.Visualize year-to-date progress toward program goals.Further insight enables your practice to: These tools can help simplify reporting and capture your practice’s performance at the patient level. Work with your PM/EMR vendor to obtain the reporting tool for QPP attestation. Clinical Quality Reporting (CQR)įor most practices, demonstrating quality care is hard enough as it is. Be sure your PM/EMR vendor can support your quality improvement initiatives and provide the reports needed, so you can measure your progress in these key areas and receive the payment you’ve earned in the process. Starting with Meaningful Use, and now with the Quality Payment Program (QPP), CMS and participating clinicians are working together to promote effective, safe, efficient, patient-centered, equitable, and timely care. The Centers for Medicare and Medicaid Services (CMS) actively incentivizes practices to meet new federal quality care standards. Make sure your practice “measures up” with these two Quality Reporting tools. Also, don’t be afraid to ask your PM/EMR vendor about their advanced reporting options. Key staff can use the reports to track every aspect of the practice’s revenue cycle. It’s imperative that your practice generate comprehensive financial reports that can demonstrate the health of the business and reveal key areas for improvement. By doing this in your practice you take the guesswork out of the appeals process, improve workflows, and reduce future denials before they occur. This helps you surface insights into why the claims were denied and to quickly address multiple charges as a group. By doing this your practice can identify hidden claims denial patterns and group them based on root causes. Implement a technology to help sniff out problem claims before they’re denied. Identifying and implementing the appropriate programs, resources and tools can help today’s medical practices right the ship and thrive in a value-based payment world. It takes more than a custom practice management configuration, and all the latest data to make sense of the practices’ cash flow and other essential data points that serve as indicators of population health. In this business climate, it’s more essential than ever to tighten the ship and have clear visibility into both clinical and financial data. Sadly, it’s increasingly difficult for practices to get paid today due to regulatory conditions and increasing burdens on patients to pay “out of pocket” for services. It’s no different when applying this to medical practices. Regardless of the industry, getting paid for services provided is a timeless hurdle. Reducing the per capita cost of providing care for a populationĬonsiderations When Targeting the Triple Aim.Improving the experience and quality of care for individuals within that population.
This revolutionary concept is known throughout healthcare and focuses on: Fast forward to today we still utilize the framework created in 2007 by IHI called the Triple Aim. Over 30 years ago a physician led group of visionaries at the Institute for Healthcare Improvement (IHI) identified the need to redesign health care.


 0 kommentar(er)
0 kommentar(er)
